Some progestogen medicines used for contraception or to manage conditions such as endometriosis have been linked to an increased risk of intracranial meningioma in a large study.
Using data from the French national health data system, researchers looked at use of eight progestogen medicines in a group of 18,061 (average age 57.6) women who had undergone intracranial meningioma surgery from 2009-18.
Compared with five times as many matched controls, and after taking account of other potentially influential factors, the researchers found that prolonged use for more than a year of three of the drugs was related to an increased risk of developing meningioma that required surgical intervention.
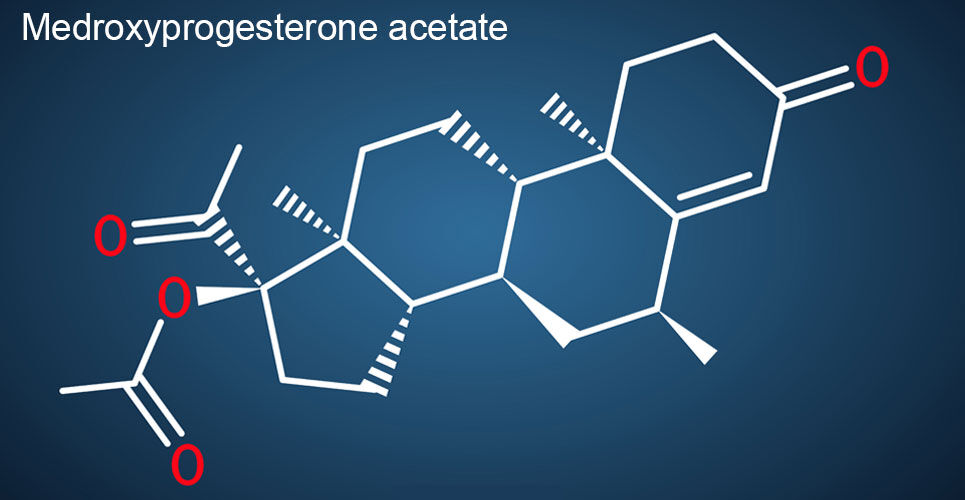
It included the contraceptive injection medroxyprogesterone acetate which was linked to a 5.6-fold higher risk, they reported in the BMJ.
Two oral pills, medrogestone and promegestone, were also associated with a 4.1- and 2.7-fold greater risk of intracranial meningioma requiring surgery respectively.
No excess risk of meningioma requiring surgery was found for progesterone, dydrogesterone or the widely used hormonal intrauterine systems, regardless of the dose of levonorgestrel they contained, the researchers said.
There also appeared to be no such risk for less than one year of use of these progestogens.
This follows other studies which had already shown a raised risk of meningioma with some high-dose progestogens but not much had been known about other more commonly used forms of the synthetic hormone, the researchers added.
As an observational study, no conclusion can be drawn around cause and effect, and there was a lack of clinical detail and medical indications for which progestogens are prescribed in the database analysed, they noted.
But ‘given that medroxyprogesterone acetate is estimated to be used for birth control by 74 million women worldwide, the number of attributable meningiomas may be potentially high,’ they said.
Further studies using other sources of data are ‘urgently needed’ to gain a better understanding of this risk, the researchers concluded.
The UK‘s Faculty of Sexual and Reproductive Health‘s Clinical Effectiveness Unit said it ‘recommends no significant change to current practice currently but does suggest that this information is included in individual discussions with patients regarding risks and benefits of various contraceptive methods‘.
And it added that it ‘will continue to monitor the evidence regarding progestogen use and the risk of meningioma‘.
NHS prescription data suggests there are around 10,000 prescriptions for medroxyprogesterone acetate every month in England.
Paul Pharoah, professor of cancer epidemiology at Cedars-Sinai Medical Centre in the US, said many of the findings in the study did not relate to UK prescriptions but there were risks around medroxyprogesterone acetate, which is sometimes used as an injectable contraception.
‘It is important to note that progestogens are an important component of many types of birth control pill (oral contraceptives) and hormone replacement therapy but there are many different types of progestogens and no association with meningioma was found for the types of progestogens commonly used in the United Kingdom,’ he said.
Professor Pharoah added that while a five-fold increase for medroxyprogesterone acetate ‘sounds like a very large risk it is important to realise that meningioma is rare and a five-fold increase in a rare disease is still a rare disease‘, and the risk would therefore need to be balanced against the benefits.
Dr Karen Noble, director of research, policy and innovation at Brain Tumour Research, said: ‘Any increased understanding of the risk factors of brain tumours is beneficial to the brain tumour community; it may open doors to research on preventative measures, as well as increase our understanding of why these tumours arise in the first place.‘
She added: ‘Although this study has linked certain progestogen treatments to an increased risk of meningioma, it has also demonstrated the safety of other progestogen treatments which were shown to not increase risk.
A version of this article was originally published by our sister publication Pulse.