Delaying, Skipping, and Altering Vaccine Schedules: Addressing Selective Vaccination
Pharmacists are poised to address selective vaccination and counsel patients contemplating delaying, skipping, or seeking an alternate vaccine schedule.
The global COVID-19 pandemic has brought the subject of vaccine confidence to the forefront, along with new interest and debate about vaccination relating to individual choice vs population health. The impact of vaccination as a milestone achievement in public health is irrefutable; nonetheless, hesitancy and skepticism regarding vaccine safety and efficacy, coupled with false or misleading health information, have rendered persisting vulnerabilities to vaccine-preventable diseases in communities and among individuals throughout the United States. The recent reemergence of polio in New York highlights the susceptibility to communicable diseases of unimmunized individuals living in communities and areas with low vaccination rates.1 Research indicates that low uptake, acceptance, and confidence in vaccines influence personal health decisions, manifesting both in parents with young children opting to follow alternative vaccination schedules and in adults opting to receive some, but not all, recommended vaccinations according to age and comorbidities. This article describes ways that pharmacists can address selective vaccination and support confidence in vaccines.
The Scope of the Issue: Vaccine Hesitancy
Vaccine hesitancy, as defined by the Strategic Advisory Group of Experts’ Working Group on Vaccine Hesitancy, is a “delay in acceptance or refusal of vaccination despite availability of vaccination services.”2 Vaccine hesitancy is as old as immunization practices themselves and certainly predates the COVID-19 pandemic; in 2019, the World Health Organization (WHO) declared vaccine hesitancy one of the top 10 threats to global health because of its potential to reverse public health gains achieved in vaccine-preventable diseases.3,4 During the COVID-19 pandemic, however, skepticism surrounding vaccines was exacerbated by social isolation and the so-called “infodemic”—the “overabundance of information, both online and offline,” resulting from viral conspiracy theories and misinformation shared across social media platforms about the SARS-CoV-2 virus and associated vaccines during the height of the pandemic in 2020.5-7
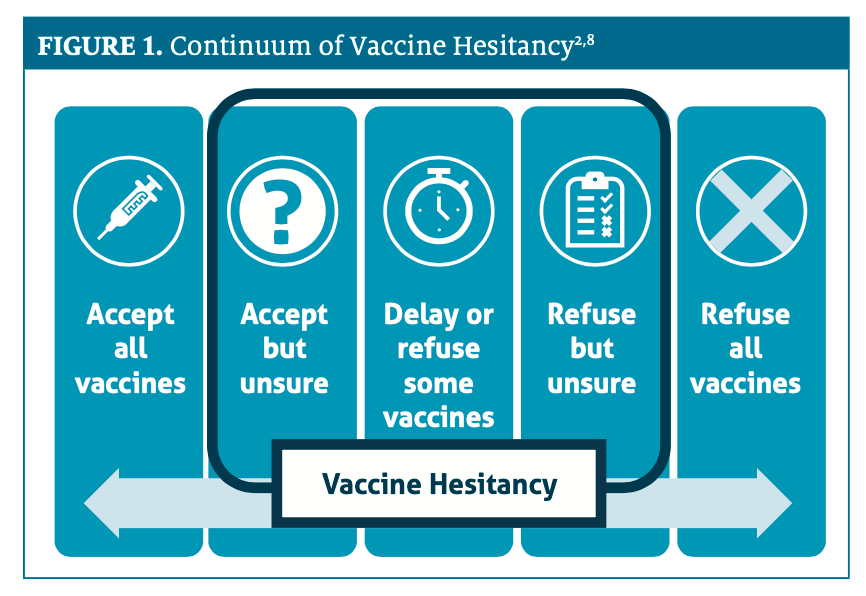
Hesitancy to receive a vaccine has been described as a “complex and context-specific” phenomenon, with time, setting, and the vaccine itself as potential variables influencing one’s decision to become immunized with a particular vaccine.2 Vaccine hesitancy and acceptance exist on a continuum of intent, with individuals often expressing varying degrees of certainty and action (Figure 1).2,8
Despite the recognition of vaccines as one of the most cost-effective preventive health care interventions,3 recent statistics related to vaccine hesitancy are striking. According to data from the Kaiser Family Foundation, more than 4 in 10 parents of children aged 6 months to 4 years (43%) indicated they will “definitely not” vaccinate their child against COVID-19. Among parents who are not vaccinated against COVID-19, 64% indicated that they will “definitely not” vaccinate their youngest children (<age 5 years). When asked for the primary reason why they will not vaccinate children under age 5 years “right away,” parents cited concerns about vaccine development (eg, newness of the vaccine, not enough testing or research), adverse events, and the overall safety of the vaccines. Survey results revealed that approximately 1 in 10 parents felt their child did not need the vaccine, or they were not worried about COVID-19.9
According to that same report, although more than three-quarters of adults in the United States have received at least 1 dose of a COVID-19 vaccine,9,10 approximately 20% indicate that they will “definitely not” receive a COVID-19 vaccine.9 Very few adults (about 4%) stated that they still might get vaccinated at some point.9 Similar to the COVID-19 vaccine experience, some communities across the United States remain vulnerable to outbreaks of vaccine-preventable diseases due to suboptimal childhood and adult vaccination rates.11,12
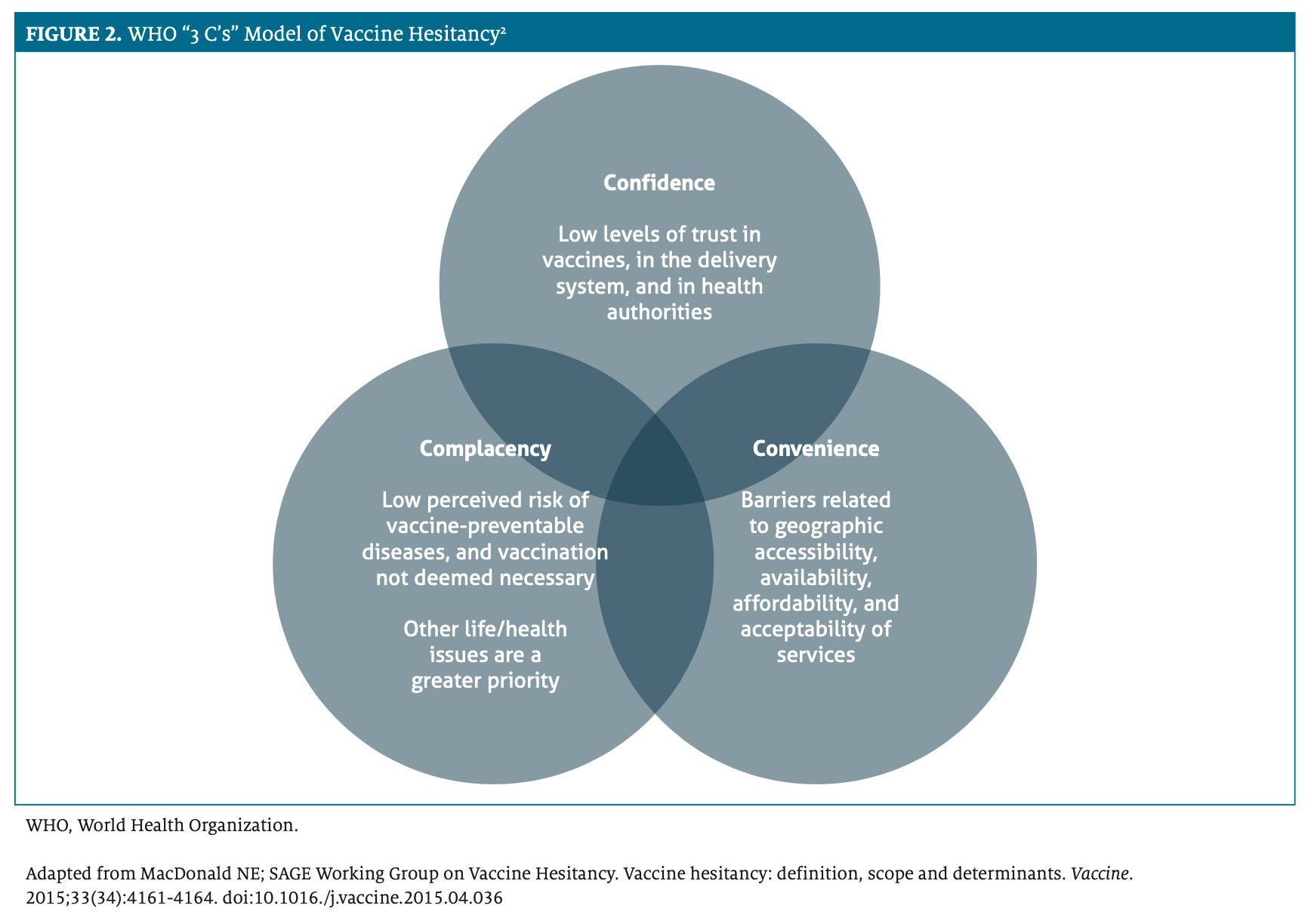
Pharmacists should recognize that vaccine hesitancy often is multifactorial; determining the reason for an individual’s hesitancy to receive a vaccine necessitates an evaluation of contributing factors and exploration of beliefs through motivational interviewing and probing, open-ended questions. The WHO 3 C’s model highlights the effects of confidence, complacency, and convenience as they relate to vaccine acceptance (Figure 2).2
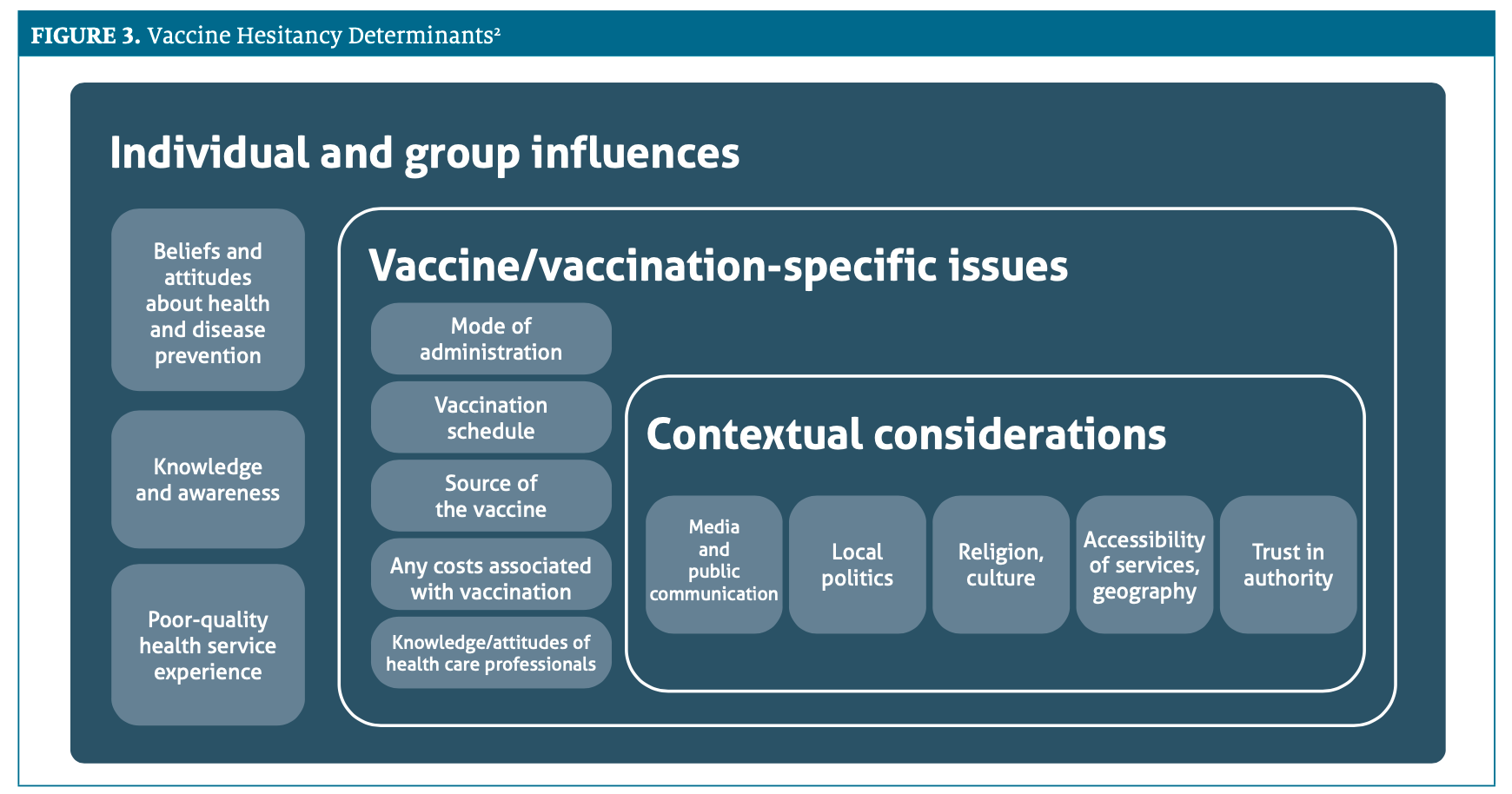
Importantly, it has been recognized that vaccine hesitancy and acceptance of vaccines—for COVID-19 and other diseases—may be based on contextual, vaccine- specific, or vaccination-specific issues, and individual and group influences (Figure 3).2
Misinformation About Delaying or Pursuing Alternative Scheduling for Immunizations
When patients ask questions about altering or delaying receipt of recommended vaccinations, pharmacists should be prepared to share information, and to direct and encourage patients to seek additional guidance from other reputable sources, including the CDC and the Advisory Committee on Immunization Practices. Some key considerations pharmacists should be prepared to address include questions and concerns related to the necessity of recommended vaccines, the need to delay or separate vaccine administration because of vaccine ingredients, or skepticism related to evidence of vaccine safety and efficacy.13
Each of these misperceptions is discussed below13,14:
- Certain vaccines are not necessary. Vaccine-preventable diseases, even if the risk of infection is perceived as rare or unlikely, are present throughout the world and, if not common in the United States, may be common elsewhere. Low or declining vaccination rates increase the risk of the rapid reemergence of vaccine-preventable diseases, as has been witnessed with recent outbreaks of measles, mumps, and polio.
- Certain vaccinations should be delayed or separated because of vaccine ingredients. Patients may ask about following alternative vaccination schedules and spacing out or separating combination vaccine products because of concerns about ingredients (eg, aluminum). There is no scientific evidence or basis that suggests accumulation in the body of a particular ingredient in a vaccine product; further, available vaccines have been tested in their final formulation, with those same ingredients and with simultaneously administered vaccines.
- Vaccines are not well tested. As with other medications and biologic products, vaccines are held to the rigorous, often decades-long development process and scientific study before approval for use by the United States Food and Drug Administration. In the case of Operation Warp Speed and the development of COVID-19 vaccines, this usually years-long process was accelerated and consolidated with multiple steps happening simultaneously and with collaboration and oversight by private corporations and government agencies in the face of an unprecedented crisis.15
Reasons to Follow the Recommended Vaccine Schedule
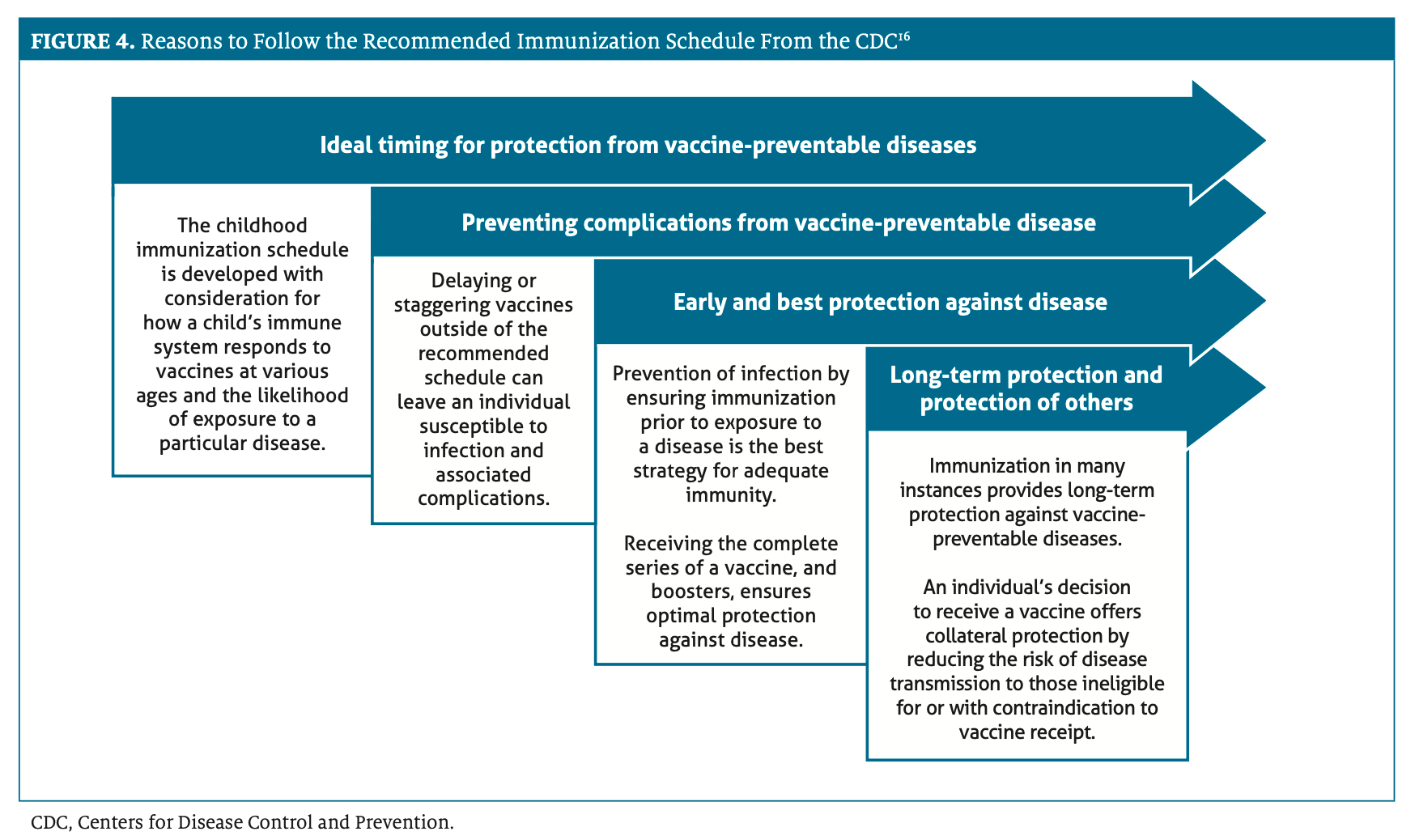
Whether for routine childhood immunizations or for adult preventive health care, pharmacists can advocate for following the recommended vaccination schedules whenever the opportunity arises. There are several reasons why adhering to the recommended vaccination schedule is appropriate, as depicted in Figure 4.16
Questions to Ask of Those Considering Modified Vaccination Schedules or Refusing Recommended Vaccinations
Pharmacists can play an important role in helping patients understand vaccination recommendations and addressing hesitancies or concerns related to a specific vaccine or vaccines. In discussing recommendations with individuals who may be contemplating delaying vaccination, seeking an alternate schedule, or refusing a particular vaccine, reasonable areas of concern to explore may include the following13,14:
- Evaluate disease fairly. Is the patient aware of their individual risk of contracting a vaccine-preventable disease and do they understand the potential risks associated with that condition? Individuals may be tempted to forgo immunizations for diseases that they perceive as less scary, deadly, or contagious. This is an opportunity to provide education on risks based on medical comorbidities, social behaviors, or age.
- Consider whether vaccine immunity is “good enough.” Are patients hesitant to receive a vaccine because of a perception that natural infection is “better” at eliciting an immune response? As seen during the COVID-19 pandemic, individuals may express a desire to forgo immunization against diseases they may perceive as being minor, less severe, not debilitating, or not life-threatening in favor of experiencing natural infection to support long-term immunity. Vaccine-induced immunity, in most cases, isadequate and bypasses the risk of severe disease, which is often unpredictable with natural infection.
- Realize the scope of “wait-and-see” approach. Is a patient choosing a “wait and see what happens to others” approach when a new vaccine becomes available instead of being vaccinated? This type of approach to immunization may render individuals who are not immunized vulnerable to infection and long-term sequela that may be potentially avoidable with early vaccination. The full risks of taking this approach should be explored and conveyed.
- Understand the importance of timing. Is there a concern, particularly regarding the childhood immunization schedule, about “overloading” the immune system or the potential effects of receiving too many vaccinations at the same time? With the pediatric immunization schedule, vaccine timing is determined relative to when an infant is most susceptible to a particular disease. In addition to consolidating immunizations into fewer office visits and ensuring earlier protection against vaccine-preventable diseases, giving multiple immunizations in combination or at a single visit may limit needle phobia and minimize trauma and stress compared with spacing out vaccinations across visits and time.
Approaches to Overcoming Barriers to Vaccine Uptake
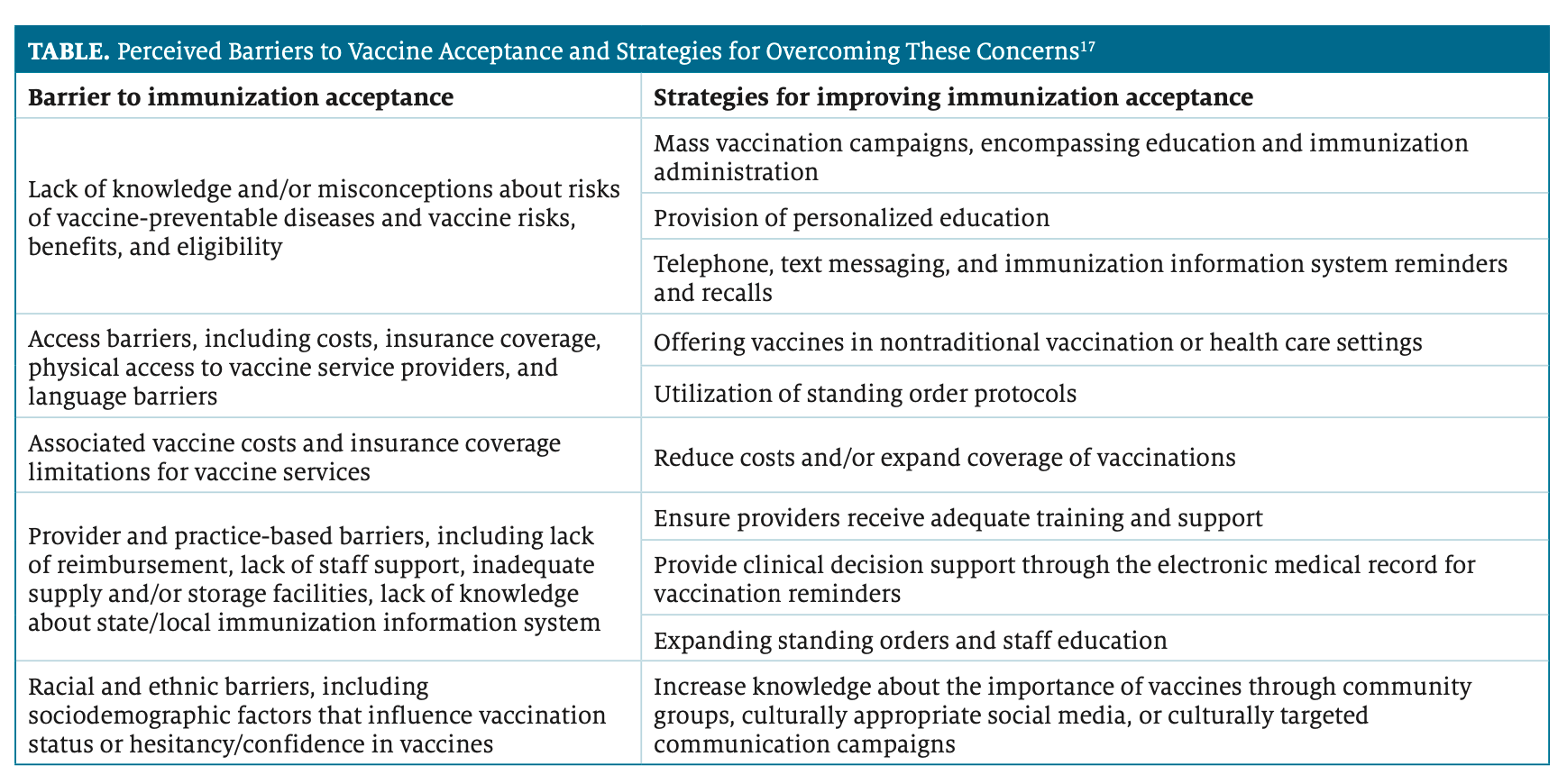
Selective vaccination and hesitancy to receive any vaccine represent barriers to achieving population-level protection against vaccine-preventable diseases. A review article by Bach et al elegantly summarized the different perceived barriers to vaccine acceptance and offered strategies for overcoming these concerns. These are included in the Table.17
Conclusions
Pharmacists are poised to address selective vaccination and counsel patients contemplating delaying, skipping, or seeking an alternate vaccine schedule. By listening to individual concerns and exploring hesitancies with compassion, pharmacists can continue to support efforts to eradicate vaccine-preventable diseases, championing greater public health for all.
About The Author
Mary Barna Bridgeman, PharmD, FCCP, BCPS, BCGP, is a clinical professor at the Ernest Mario School of Pharmacy at Rutgers University and an internal medicine clinical pharmacist at Robert Wood Johnson University Hospital, both in New Brunswick, New Jersey.
References
1. Link-Gelles R, Lutterloh E, Schnabel Ruppert P, et al; 2022 U.S.
Poliovirus Response Team. Public health response to a case of paralytic poliomyelitis in an unvaccinated person and detection of poliovirus in wastewater — New York, June-August 2022. MMWR Morb Mortal Wkly Rep. 2022;71(33):1065-1068. doi:10.15585/mmwr.mm7133e2
2. MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4164. doi:10.1016./j.vaccine.2015.04.036
3. Ten threats to global health in 2019. World Health Organization. Accessed August 20, 2022. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
4. Schwartz JL. New media, old messages: themes in the history of vaccine hesitancy and refusal. Virtual Mentor. 2012;14(1):50-55. doi:10.1001/virtualmentor.2012.14.1.mhst1-1201
5. Munich Security Conference. World Health Organization. February 15, 2020. Accessed August 1, 2022. http://www.who.int/director-general/speeches/detail/munich-security-conference
6. Managing the COVID-19 infodemic: promoting healthy behaviours and mitigating the harm from misinformation and disinformation. Joint statement by WHO, UN, UNICEF, UNDP, UNESCO, UNAIDS, ITU, UN Global Pulse, and IFRC. World Health Organization. September 23, 2020. Accessed September 16, 2022. https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation
7. Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28(3):456-459. doi:10.1038/s41591-022-01728-z
8. Overhage JM, Agrawal S. COVID-19 vaccination perceptions among socially vulnerable Medicare and Medicaid members: experience from a national health plan outreach program. July 29, 2021. Accessed August 1, 2022. https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0162
9. COVID Data Tracker. CDC. Updated September 14, 2022. Accessed September 16, 2022. https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-additional-dose-totalpop
10. Lopes L, Hamel L, Sparks G, Montero A, Presiado M, Brodie M. KFF COVID-19 vaccine monitor: July 2022. Accessed August 1, 2022. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine- monitor-july-2022/
11. Vaccination coverage among young children (0 – 35 months). CDC. Updated September 28, 2020. Accessed August 20, 2022. https://www.cdc.gov/vaccines/imz-managers/coverage/childvaxview/interactive-reports/ index.html
12. Vaccination coverage among adults. CDC. Updated May 14, 2021. Accessed August 20, 2022. https://www.cdc.gov/vaccines/imz-managers/coverage/ adultvaxview/data-reports/general-population/index.html
13. When individual doctors make their own immunization schedules: what you should know. Children’s Hospital of Philadelphia Vaccine Education Center. Fall 2017. Accessed August 20, 2022. https://media.chop.edu/data/files/pdfs/vec-individual-doctors-vaccine-schedule.pdf
14. Vaccine schedule: altering the schedule. Children’s Hospital of Philadelphia. Updated September 6, 2022. Accessed September 16, 2022. https://www.chop.edu/centers-programs/vaccine-education-center/vaccine-schedule/altering-the-schedule
15. Explaining Operation Warp Speed. U.S. Department of Health & Human Services. Accessed September 16, 2022. https://www.nihb.org/covid-19/wp- content/uploads/2020/08/Fact-sheet-operation-warp-speed.pdf
16. Reasons to follow CDC’s recommended immunization schedule. CDC. Updated February 25, 2020. Accessed August 20, 2022. https://www.cdc.gov/vaccines/parents/schedules/reasons-follow-schedule.html
17. Bach AT, Kang AY, Lewis J, Xavioer S, Portillo I, Goad JA. Addressing common barriers in adult immunizations: a review of interventions. Expert Rev Vaccines. 2019;18(11):1167-1185. doi:10.1080/14760584.2019.1698955