Key takeaways
Medication side effects can cause drowsiness, vision changes, impaired motor skills, delayed reaction time, and a lack of focus, which are dangerous when operating a vehicle.
Opioids and other prescription pain relievers, anxiety medications, antidepressants, anticonvulsants, antihistamines, sedatives, stimulants, and muscle relaxants are some common medications that can impair drivers.
Medication-related car accidents are preventable by talking to your doctor, reading medication labels, understanding side effects, and planning ahead for safe transportation.
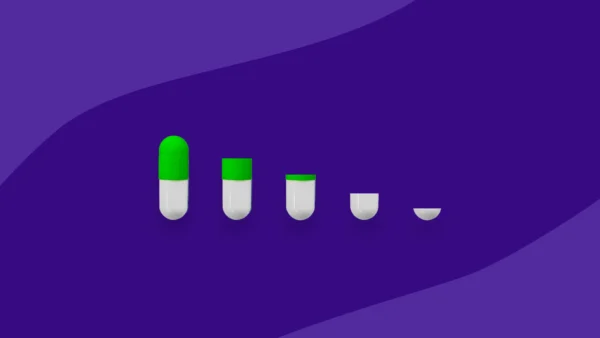
Most people know the risks of driving under the influence of alcohol, but many are unaware of how certain medications can affect their driving abilities. Prescription side effects can cause drowsiness, vision changes, impaired motor skills, delayed reaction time, and even lack of focus—all of which are dangerous when operating a vehicle.
Given the various ways medications can impair driving, it’s crucial to understand how the substances in your system may affect your ability to drive safely.
How do medications affect driving?
Medications can have various side effects, which is why patients are often told not to consume alcohol or operate a vehicle after taking them. Patients should carefully review medication labels and consult healthcare professionals to understand potential side effects before driving.
Drowsiness, delayed reaction times, and vision impairment are just a few side effects of medications that can impact driving performance. Awareness of each medication’s impact is critical when deciding whether it is safe to drive.
Drowsiness or fainting
The risk of drowsiness or fainting due to medication poses a significant risk. Many prescription drugs can cause dizziness or lightheadedness (like benzodiazepines), particularly those that cause dehydration (as seen with antihistamines) or low blood sugar (associated with beta blockers). These effects increase the risk of accidents, particularly among older adults.
Research indicates there is a correlation between the number of medications taken and the likelihood of traffic accidents — a major contributor to injuries and fatalities. It is essential to understand the difference between drowsiness and dizziness. Dizziness refers to feeling unsteady, lightheaded, or experiencing a sensation of spinning. Drowsiness denotes a state of feeling sleepily fatigued, leading to a reduced level of alertness.
Dizziness
Medications that lead to dizziness are of critical concern in the context of driving. Examples of medicines that have this effect include anticonvulsants, antidepressants, muscle relaxers, blood pressure medications, pain relievers like hydrocodone (an opioid), over-the-counter ibuprofen and naproxen, sleeping pills, and nitroglycerin.
The potential impairment caused by these medications underscores the importance of heightened awareness among current drivers, driving educators, and new drivers to ensure road safety.
Vision changes
Some medications may lead to side effects such as blurred vision or heightened sensitivity to light, resulting in significant challenges while driving.
Noteworthy medications known for impacting eyesight include alendronate (Fosamax), isotretinoin (Accutane), topiramate (Topamax), tamsulosin (Flomax), amiodarone (Cordarone), tamoxifen, sildenafil (Viagra), and rifampin (Rifadin).
It’s important to clarify that this list isn’t exhaustive, which emphasizes the importance of checking medication side effects before driving. If a medication explicitly advises against driving, adhering to this guidance is a non-negotiable for ensuring road safety.
Impaired motor skills
Driving is a multifaceted activity, demanding cognitive, motor, and visual coordination. All three of these functions are essential for safe navigation on the road. However, introducing certain medications can disrupt this balance by impairing motor skills and compromising your capability to maintain control of a vehicle.
Medications with the potential to impair motor skills may affect coordination and control, increasing the risk of accidents. Some medications (including muscle relaxants, antispasmodics, and drugs affecting neuromuscular transmission) may result in impaired muscle coordination and weakness. This may cause issues while driving, such as difficulty maintaining a firm grip on the steering wheel or manipulating the vehicle’s controls.
When taking medications, you should be aware of how each of your medications may affect your motor abilities. Responsible driving may include adjusting habits or finding alternative means of transportation.
Delayed reaction times
Your reaction time—the moment between recognizing a hazard and deciding what to do—precedes your vehicle’s mechanical actions. Some medications delay this process, leading to potential safety issues while driving.
The combination of reaction time, thinking time, thinking distance, and braking time and distance leads to an average time to stop a vehicle of 6.5 seconds. This includes a one-second delay in your reaction time and a 2.5-second delay in applying the brakes. This means that, depending on the vehicle’s speed, you may require a distance of 302 feet (92 meters) to come to a complete stop.
Medications that depress the central nervous system (like sedatives, opioids, and other depressants) may lead to a slower reaction time. This may be problematic in situations where quick responses are necessary, such as when braking suddenly or avoiding obstacles.
Lack of focus on the road
Annually, around 3,000 lives are lost in car accidents attributed to distracted driving, which constitutes 8% to 9% of all fatal motor vehicle collisions in the U.S. or nine lives daily.
Some drugs contribute to a lack of focus by impairing attention and concentration while on the road. Medications commonly associated with this side effect include anti-anxiety medications, tricyclic antidepressants, sleep aids, and antiseizure drugs. In addition, drugs that induce brain fog significantly contribute to distracted driving.
What medications may affect driving?
Driving safely requires a sharp mind and focused attention, but certain medications can significantly impact one’s ability behind the wheel. From opioids causing dizziness to benzodiazepines compromising vehicle operation, various medications pose risks on the road.
Opioids and other pain medications
Opioids (a class of pain medications) include morphine, oxycodone, and hydrocodone. These can affect the central nervous system, causing dizziness, sleepiness, and mood changes, which have implications for driving safety.
Caution when taking such drugs is critical because these side effects can negatively impact psychomotor and mental performance. It’s essential when taking opioids to be aware of these potential effects and exercise heightened caution when driving.
Anxiety medications
Anti-anxiety medications, designed to alleviate symptoms like panic attacks, include benzodiazepines. This medication group also promotes better sleep. However, it’s important to exercise caution when driving under the influence of benzodiazepines because these drugs can compromise the safe operation of a vehicle. Common benzodiazepines include Xanax (alprazolam), Ativan (lorazepam), Klonopin (clonazepam), and Restoril (temazepam).
These medications may increase the risk of a crash, particularly when combined with alcohol or other sedatives. The risk is highest when you first start using benzodiazepines before you’ve become accustomed to their effects.
Antidepressants
Approximately 1 in 10 Americans aged 12 and older rely on antidepressant medication for relief from depression symptoms. However, side effects like drowsiness, hypotension, suicidal ideation, dizziness, decreased seizure threshold, nausea, and anxiety are common.
These effects may interfere with driving abilities. When taking antidepressants, you should be aware of these side effects to ensure a balance between mental health management and responsible road use.
There are five common types of antidepressants:
- Selective serotonin reuptake inhibitors (SSRIs) such as Zoloft (sertraline), Prozac (fluoxetine), Celexa (citalopram), Lexapro (escitalopram), and Paxil (paroxetine)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs) such as Cymbalta (duloxetine) and Effexor (venlafaxine)
- Tricyclic antidepressants (TCAs) such as Tofranil (imipramine) and Elavil (amitriptyline).
- Monoamine oxidase inhibitors (MAOIs) such as Marplan (isocarboxazid), Nardil (phenelzine), Emsam (selegiline), and Parnate (tranylcypromine)
- Tricyclic antidepressants such as Tofranil (imipramine), Pamelor (nortriptyline), Elavil (amitriptyline), Sinequan (doxepin) and Norpramin (desipramine)
Atypical antidepressants include Wellbutrin (Bupropion), Remeron (mirtazapine), Trazodone, Viibryd (vilazodone), and Trintellix (vortioxetine).
Seizure medications
Seizure medications are vital for controlling epilepsy but may impact driving safety by causing slower reactions, unsteadiness, and various other side effects.
Common seizure medications include Klonopin (clonazepam), Neurontin (gabapentin), Lamictal (lamotrigine), Ativan (lorazepam), Topamax (topiramate), and Depakote (valproic acid).
Antihistamines
Antihistamines are frequently used to alleviate allergy symptoms. They work by targeting excessive histamine production by the body’s immune system. As well as treating allergies to pollen and other triggers, antihistamines are useful for stomach problems and colds. However, it’s important to exercise caution when driving under the influence of antihistamines, as they can cause drowsiness, impaired reaction times, blurred vision, and mild confusion.
Antihistamines have differing levels of side effects, as some cause drowsiness and some do not. Antihistamines with drowsy side effects include chlorphenamine, cinnarizine, diphenhydramine, hydroxyzine, and promethazine. Non-drowsy antihistamines include acrivastine, cetirizine, fexofenadine, and loratadine. However, it’s important to note that “non-drowsy” antihistamines impact everybody differently and may have sedating effects. It’s important to know how medications impact you before you get behind the wheel.
Sleep medications and sedatives
Sleep medications and sedatives (common for insomnia relief) have delayed effects that may result in slow reaction times and impaired judgment. A study by the Sleep Research Society found a positive association between nighttime (insomnia and short sleep) and daytime (sleepiness and fatigue) symptoms with reports of car accidents. Participants using over-the-counter sleep medications were 41.9% more likely to report a road collision. Sedatives can heighten crash risks by influencing judgment regarding vehicle operation and increasing drowsiness. In rare occasions when taking sleep medications like Ambien (zolpidem), parasomnias such as sleepwalking and sleep-driving can coexist.
Stimulants
Stimulants such as Adderall (amphetamine/dextroamphetamine), Ritalin and Concerta (methylphenidate), Dexedrine (dextroamphetamine), and Vyvanse (lisdexamfetamine) may profoundly affect driving performance. Whereas these substances might provide users with a sense of well-being, this is often accompanied by difficulty concentrating, impatience, aggressiveness, and chronic paranoia. This altered mental state poses significant risks on the road, contributing to erratic behavior and creating dangerous driving situations.
Muscle relaxants
Muscle relaxants, prescribed for symptoms like spasms and musculoskeletal pain, impact muscle function. The two major classes (anti-spastics and antispasmodics) have distinct uses and side effects. However, both impact muscle function, motor skills, and coordination and can cause drowsiness by affecting the central nervous system.
Common antispasmodic medications include Flexeril (cyclobenzaprine), Skelaxin (metaxalone), Robaxin (methocarbamol), Norflex (orphenadrine), Vanadom (carisoprodol), and Lorzone (chlorzoxazone).
Common antispastic medications include Dantrium (dantrolene) and Lioresal (Baclofen).
Two medications that have both antispasmodic and antispastic effects are Valium (diazepam) and Zanaflex (tizanidine).
While muscle relaxants primarily target muscle function, their effects on the central nervous system can lead to sedation, drowsiness, and impaired cognitive function, all of which can compromise your ability to drive safely. It’s important while taking muscle relaxants to be aware of these potential side effects and to exercise caution when driving, particularly until you understand how the medication affects you personally. Consulting with a healthcare provider about medication use and driving safety is advisable.
How to prevent medication-related road accidents
Preventing medication-related road accidents relies on proactive measures. Talk to your healthcare providers or pharmacist to understand the driving-related side effects of any medications you take.
In addition, you should read labels carefully, understand medication interactions, and plan for safe transportation.
Talk to your healthcare provider and pharmacist
Discussing your medications with your healthcare providers will enable them to find a treatment plan that has minimal impact on your driving abilities. Openly share your concerns and experiences to receive personalized guidance.
Read medication labels
Understanding the labels on your prescription medications is crucial. This will ensure you take your medicine correctly, as recommended in your treatment plan.
Regular review of medication labels and open communication with your healthcare providers is essential to stay updated on any changes in your prescriptions and maintain a balance between effective treatment and road safety.
Understand medication side effects
Taking the time to understand possible drug side effects will prepare you to mitigate or cope with any effects.
Side effects can vary in onset and duration. Some medications show immediate effects, while others take time. Before driving after taking these medications, consider their characteristics and potential impact on cognitive and motor functions. Not everyone may experience side effects affecting driving. Consult your healthcare provider for personalized guidance and monitor your responses to medications.
Plan ahead for safe transportation
Planning for safe transportation has never been easier. Using rideshare services like Uber and Lyft offers a convenient alternative to driving. Calling family or friends for a ride could be another option. Finding out about public transportation options in your area could also provide you with greater flexibility.
Risks of driving while impaired
Understanding the impact of medications on driving safety is crucial for preventing harm to yourself and others and for avoiding legal consequences.
Although field sobriety and breathalyzer tests can detect alcohol, identifying medication impairment poses a challenge. However, if law enforcement does a toxicology screening and finds traces of prescription or over-the-counter drugs in your system that may have affected your ability to drive, you may receive a DUI with drug charges. Signs like weaving between lanes, speeding, or running red lights may indicate impairment.
FAQ
What should I do if I have to take my medication but also need to drive?
If you need to take medication and drive, consult your healthcare provider to determine the optimal time for medication to minimize driving risks. Additionally, explore alternative transportation options to ensure safety on the road. Communicating with your healthcare provider will help you establish a medication plan that aligns with your driving needs.
Is it illegal to drive while on medication?
Whether driving on medication is illegal depends on the specific medication. Although many medications don’t impact driving, some prescription and over-the-counter drugs can cause side effects like sleepiness, blurred vision, and dizziness, making it unsafe to drive.
Understanding the potential side effects and seeking alternatives ensures responsible and legal road practices.
Sources
- Impact of medical conditions and medications on road traffic safety, Oman Medical Journal (2018)
- Drugs that might be the cause of your dizziness, Consumer Reports (2017)
- Vision and medications: what medications can affect your vision, ADV Vision (2020)
- When driving, what is the average reaction time, J.D. Power (2023)
- Distracted driving statistics & facts in 2024, Forbes (2023)
- Caution! These drugs can cause memory loss, AARP (2023)
- Driving under the influence of opioids: What prescribers should know, Journal of Opioid Management (2018)
- Antidepressant use in persons aged 12 and over, CDC (2011)
- Depression, antidepressants and driving safety, Injury Epidemiology (2017)
- Epilepsy, antiepilepsy drugs, and serious car crashes, Neurology (2018)
- Some medicines and driving don’t mix, FDA (2021)
- Insomnia, hypnotic use, and road collisions, Oxford academic (2020)
- Finding and learning about side effects (adverse reactions), FDA (2022)
- Prescription Medication Usage and Crash Culpability in a Population of Injured Drivers, NIH (2011)
- Medication use and the risk of motor vehicle collisions among licensed drivers: A systematic review, NIH (2017)